Drug Detail:Savaysa (Edoxaban [ e-dox-a-ban ])
Drug Class: Factor Xa inhibitors
Highlights of Prescribing Information
SAVAYSA (edoxaban) tablets, for oral use
Initial U.S. Approval: 2015
WARNING: (A) REDUCED EFFICACY IN NONVALVULAR ATRIAL FIBRILLATION PATIENTS WITH CREATININE CLEARANCE (CRCL) > 95 ML/MIN (B) PREMATURE DISCONTINUATION OF SAVAYSA INCREASES THE RISK OF ISCHEMIC EVENTS (C) SPINAL/EPIDURAL HEMATOMA
See full prescribing information for complete boxed warning.
(A) REDUCED EFFICACY IN NONVALVULAR ATRIAL FIBRILLATION PATIENTS WITH CRCL > 95 ML/MIN: SAVAYSA should not be used in patients with CrCL > 95 mL/min. In the ENGAGE AF-TIMI 48 study, nonvalvular atrial fibrillation patients with CrCL > 95 mL/min had an increased rate of ischemic stroke with SAVAYSA 60 mg once daily compared to patients treated with warfarin. In these patients another anticoagulant should be used (5.1).
(B) PREMATURE DISCONTINUATION OF SAVAYSA INCREASES THE RISK OF ISCHEMIC EVENTS: Premature discontinuation of any oral anticoagulant in the absence of adequate alternative anticoagulation increases the risk of ischemic events. If SAVAYSA is discontinued for a reason other than pathological bleeding or completion of a course of therapy, consider coverage with another anticoagulant as described in the transition guidance (2.4, 5.2, 14).
(C) SPINAL/EPIDURAL HEMATOMA: Epidural or spinal hematomas may occur in patients treated with SAVAYSA who are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis. Consider these risks when scheduling patients for spinal procedures (5.4).
Recent Major Changes
| Warnings and Precautions, Increased Risk of Thrombosis in Patients with Triple Positive Antiphospholipid Syndrome (5.6) | 04/2020 |
Indications and Usage for Savaysa
SAVAYSA is a factor Xa inhibitor indicated:
To reduce the risk of stroke and systemic embolism (SE) in patients with nonvalvular atrial fibrillation (NVAF) (1.1)
-
Limitation of Use for NVAF
SAVAYSA should not be used in patients with creatinine clearance (CrCL) > 95 mL/min because of increased risk of ischemic stroke compared to warfarin at the highest dose studied (60 mg) (1.1)
SAVAYSA is indicated for the treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE) following 5 to 10 days of initial therapy with a parenteral anticoagulant (1.2)
Savaysa Dosage and Administration
-
Treatment of NVAF:
Assess CrCL before initiating therapy (2.1)
The recommended dose is 60 mg once daily in patients with CrCL >50 to ≤ 95 mL/min. Do not use SAVAYSA in patients with CrCL > 95 mL/min (2.1)
Reduce dose to 30 mg once daily in patients with creatinine clearance 15 to 50 mL/min (2.1)
-
Treatment of DVT and PE:
The recommended dose is 60 mg once daily (2.2)
Reduce dose to 30 mg once daily for patients with CrCL 15 to 50 mL/min or body weight less than or equal to 60 kg or who use certain P-gp inhibitors (2.2)
Dosage Forms and Strengths
Tablets: 60 mg, 30 mg, and 15 mg (3)
Contraindications
- Active pathological bleeding (4)
Warnings and Precautions
- Bleeding: Serious and potentially fatal bleeding. Promptly evaluate signs and symptoms of blood loss (5.3)
- Mechanical Heart Valves or Moderate to Severe Mitral Stenosis: Use is not recommended (5.5)
- Increased Risk of Thrombosis in Patients with Triple Positive Antiphospholipid Syndrome: SAVAYSA use not recommended. (5.6)
Adverse Reactions/Side Effects
Treatment of NVAF: The most common adverse reactions (≥ 5%) are bleeding and anemia (6.1)
Treatment of DVT and PE: The most common adverse reactions (≥ 1%) are bleeding, rash, abnormal liver function tests and anemia (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Daiichi Sankyo, Inc. at 1-877-437-7763 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Anticoagulants, Antiplatelets, Thrombolytics, and Selective Serotonin Reuptake Inhibitors (SSRIs)/Serotonin Norepinephrine Reuptake Inhibitors (SNRIs): Avoid concomitant use due to increased risk of bleeding. (7.1)
- Rifampin: Avoid concomitant use (7.2)
Use In Specific Populations
- Lactation: Advise not to breastfeed. (8.2)
- Impaired renal function (CrCL 15 to 50 mL/min): Reduce dose (2.1, 2.2, 8.6)
- Moderate or severe hepatic impairment: Not recommended (8.7)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 3/2021
Full Prescribing Information
WARNING: (A) REDUCED EFFICACY IN NONVALVULAR ATRIAL FIBRILLATION PATIENTS WITH CREATININE CLEARANCE (CRCL) > 95 ML/MIN (B) PREMATURE DISCONTINUATION OF SAVAYSA INCREASES THE RISK OF ISCHEMIC EVENTS (C) SPINAL/EPIDURAL HEMATOMA
1. Indications and Usage for Savaysa
2. Savaysa Dosage and Administration
2.1 Nonvalvular Atrial Fibrillation
The recommended dose of SAVAYSA is 60 mg taken orally once daily [see Warnings and Precautions (5.1) and Clinical Studies (14.1)]. Assess creatinine clearance, as calculated using the Cockcroft-Gault equation1, before initiating therapy with SAVAYSA. Do not use SAVAYSA in patients with CrCL > 95 mL/min.
Reduce SAVAYSA dose to 30 mg once daily in patients with CrCL 15 to 50 mL/min [see Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
- 1
- Cockcroft-Gault CrCL = (140-age) × (weight in kg) × (0.85 if female) / (72 × creatinine in mg/dL).
2.2 Treatment of Deep Vein Thrombosis and Pulmonary Embolism
The recommended dose of SAVAYSA is 60 mg taken orally once daily following 5 to 10 days of initial therapy with a parenteral anticoagulant [see Clinical Studies (14.2)].
Reduce SAVAYSA dose to 30 mg once daily in patients with CrCL 15 to 50 mL/min, patients who weigh less than or equal to 60 kg, or patients who are taking certain concomitant P-gp inhibitor medications [see Clinical Studies (14.2)].
2.3 Administration Information
If a dose of SAVAYSA is missed, the dose should be taken as soon as possible on the same day. Dosing should resume the next day according to the normal dosing schedule. The dose should not be doubled to make up for a missed dose.
SAVAYSA can be taken without regard to food [see Clinical Pharmacology (12.3)].
2.4 Transition to or from SAVAYSA
| From | To | Recommendation |
|---|---|---|
| Warfarin or other Vitamin K Antagonists | SAVAYSA | Discontinue warfarin and start SAVAYSA when the INR is ≤ 2.5 |
| Oral anticoagulants other than warfarin or other Vitamin K Antagonists | SAVAYSA | Discontinue current oral anticoagulant and start SAVAYSA at the time of the next scheduled dose of the other oral anticoagulant |
| Low Molecular Weight Heparin (LMWH) | SAVAYSA | Discontinue LMWH and start SAVAYSA at the time of the next scheduled administration of LMWH |
| Unfractionated heparin | SAVAYSA | Discontinue the infusion and start SAVAYSA 4 hours later |
| From | To | Recommendation |
|---|---|---|
| Abbreviations: INR=International Normalized Ratio | ||
| SAVAYSA | Warfarin | Oral option: For patients taking 60 mg of SAVAYSA, reduce the dose to 30 mg and begin warfarin concomitantly. For patients receiving 30 mg of SAVAYSA, reduce the dose to 15 mg and begin warfarin concomitantly. INR must be measured at least weekly and just prior to the daily dose of SAVAYSA to minimize the influence of SAVAYSA on INR measurements. Once a stable INR ≥ 2.0 is achieved, SAVAYSA should be discontinued and the warfarin continued |
| SAVAYSA | Warfarin | Parenteral option: Discontinue SAVAYSA and administer a parenteral anticoagulant and warfarin at the time of the next scheduled SAVAYSA dose. Once a stable INR ≥ 2.0 is achieved the parenteral anticoagulant should be discontinued and the warfarin continued |
| SAVAYSA | Non-Vitamin-K-Dependent Oral anticoagulants | Discontinue SAVAYSA and start the other oral anticoagulant at the time of the next dose of SAVAYSA |
| SAVAYSA | Parenteral anticoagulants | Discontinue SAVAYSA and start the parenteral anticoagulant at the time of the next dose of SAVAYSA |
2.5 Discontinuation for Surgery and Other Interventions
Discontinue SAVAYSA at least 24 hours before invasive or surgical procedures because of the risk of bleeding [see Warnings and Precautions (5.3)].
If surgery cannot be delayed, there is an increased risk of bleeding. This risk of bleeding should be weighed against the urgency of intervention [see Warnings and Precautions (5.3)].
SAVAYSA can be restarted after the surgical or other procedure as soon as adequate hemostasis has been established noting that the time to onset of pharmacodynamic effect is 1-2 hours [see Warnings and Precautions (5.2)]. Administer a parenteral anticoagulant and then switch to oral SAVAYSA, if oral medication cannot be taken during or after surgical intervention.
2.6 Administration Options
For patients who are unable to swallow whole tablets, SAVAYSA tablets may be crushed and mixed with 2 to 3 ounces of water and immediately administered by mouth or through a gastric tube. The crushed tablets may also be mixed into applesauce and immediately administered orally [see Clinical Pharmacology (12.3)].
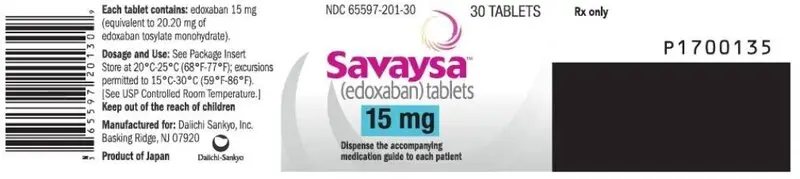
3. Dosage Forms and Strengths
- 60 mg, yellow round shaped, film-coated tablets, debossed with DSC L60 on one side
- 30 mg, pink round shaped, film-coated tablets, debossed with DSC L30 on one side
- 15 mg, orange round shaped, film-coated tablets, debossed with DSC L15 on one side
4. Contraindications
SAVAYSA is contraindicated in patients with:
- Active pathological bleeding [see Warnings and Precautions (5.3) and Adverse Reactions (6.1)].
5. Warnings and Precautions
5.1 Reduced Efficacy in Nonvalvular Atrial Fibrillation Patients with CrCL > 95 mL/min
SAVAYSA should not be used in patients with CrCL > 95 mL/min. In the randomized ENGAGE AF-TIMI 48 study, NVAF patients with CrCL > 95 mL/min had an increased rate of ischemic stroke with SAVAYSA 60 mg daily compared to patients treated with warfarin. In these patients another anticoagulant should be used [see Dosage and Administration (2.1) and Clinical Studies (14.1)].
5.2 Increased Risk of Stroke with Discontinuation of SAVAYSA in Patients with Nonvalvular Atrial Fibrillation
Premature discontinuation of any oral anticoagulant in the absence of adequate alternative anticoagulation increases the risk of ischemic events. If SAVAYSA is discontinued for a reason other than pathological bleeding or completion of a course of therapy, consider coverage with another anticoagulant as described in the transition guidance [see Dosage and Administration (2.4) and Clinical Studies (14.1)].
5.3 Risk of Bleeding
SAVAYSA increases the risk of bleeding and can cause serious and potentially fatal bleeding. Promptly evaluate any signs or symptoms of blood loss.
Discontinue SAVAYSA in patients with active pathological bleeding.
Concomitant use of drugs affecting hemostasis may increase the risk of bleeding. These include aspirin and other antiplatelet agents, other antithrombotic agents, fibrinolytic therapy, chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs), selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) [see Drug Interactions (7.1)].
5.4 Spinal/Epidural Anesthesia or Puncture
When neuraxial anesthesia (spinal/epidural anesthesia) or spinal/epidural puncture is employed, patients treated with antithrombotic agents for prevention of thromboembolic complications are at risk of developing an epidural or spinal hematoma, which can result in long-term or permanent paralysis.
The risk of these events may be increased by the postoperative use of indwelling epidural catheters or the concomitant use of medicinal products affecting hemostasis. Indwelling epidural or intrathecal catheters should not be removed earlier than 12 hours after the last administration of SAVAYSA. The next dose of SAVAYSA should not be administered earlier than 2 hours after the removal of the catheter. The risk may also be increased by traumatic or repeated epidural or spinal puncture.
Monitor patients frequently for signs and symptoms of neurological impairment (e.g., numbness or weakness of the legs, bowel, or bladder dysfunction). If neurological compromise is noted, urgent diagnosis and treatment is necessary. Prior to neuraxial intervention the physician should consider the potential benefit versus the risk in anticoagulated patients or in patients to be anticoagulated for thromboprophylaxis.
5.5 Patients with Mechanical Heart Valves or Moderate to Severe Mitral Stenosis
The safety and efficacy of SAVAYSA has not been studied in patients with mechanical heart valves or moderate to severe mitral stenosis. The use of SAVAYSA is not recommended in these patients [see Clinical Studies (14.1)].
5.6 Increased Risk of Thrombosis in Patients with Triple Positive Antiphospholipid Syndrome
Direct-acting oral anticoagulants (DOACs), including SAVAYSA, are not recommended for use in patients with triple positive antiphospholipid syndrome (APS). For patients with APS (especially those who are triple positive [positive for lupus anticoagulant, anticardiolipin antibodies, and anti-beta 2-glycoprotein I antibodies]), treatment with DOACs has been associated with increased rates of recurrent thrombotic events compared with vitamin K antagonist therapy.
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are discussed in greater detail in other sections of the prescribing information.
- Increased Risk of Stroke with Discontinuation of SAVAYSA in Patients with Nonvalvular Atrial Fibrillation [see Warnings and Precautions (5.2)]
- Risk of Bleeding [see Warnings and Precautions (5.3)]
- Spinal/Epidural Anesthesia or Puncture [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of SAVAYSA was evaluated in the ENGAGE AF-TIMI 48, Hokusai VTE, and Hokusai VTE Cancer studies including 11,530 patients exposed to SAVAYSA 60 mg and 7124 patients exposed to SAVAYSA 30 mg once daily [see Clinical Studies (14)].
The ENGAGE AF-TIMI 48 Study
In the ENGAGE AF-TIMI 48 study, the median study drug exposure for the SAVAYSA and warfarin treatment groups was 2.5 years.
Bleeding was the most common reason for treatment discontinuation. Bleeding led to treatment discontinuation in 3.9% and 4.1% of patients in the SAVAYSA 60 mg and warfarin treatment groups, respectively.
In the overall population, major bleeding was lower in the SAVAYSA group compared to the warfarin group [HR 0.80 (0.70, 0.91), p < 0.001]. Table 6.1 shows major bleeding events (percentage of patients with at least one bleeding event, per year) for the indicated population (CrCL ≤ 95 mL/min).
| Event† | SAVAYSA 60 mg‡
N = 5417 n (%/year) | Warfarin N = 5485 n (%/year) | SAVAYSA 60 mg vs. Warfarin HR (95% CI) |
|---|---|---|---|
| Abbreviations: HR = Hazard Ratio versus Warfarin, CI = Confidence Interval, n = number of patients with events, N = number of patients in Safety population, | |||
|
|||
| Major Bleeding§ | 357 (3.1) | 431 (3.7) | 0.84 (0.73, 0.97) |
| Intracranial Hemorrhage (ICH)¶ | 53 (0.5) | 122 (1.0) | 0.44 (0.32, 0.61) |
| Hemorrhagic Stroke | 33 (0.3) | 69 (0.6) | 0.49 (0.32, 0.74) |
| Other ICH | 20 (0.2) | 55 (0.5) | 0.37 (0.22, 0.62) |
| Gastrointestinal# | 205 (1.8) | 150 (1.3) | 1.40 (1.13, 1.73) |
| Fatal BleedingÞ | 21 (0.2) | 42 (0.4) | 0.51 (0.30, 0.86) |
| ICH | 19 (0.2) | 36 (0.3) | 0.54 (0.31, 0.94) |
| Non-intracranial | 2 (< 0.1) | 6 (< 0.1) | ---- |
The most common site of a major bleeding event was the gastrointestinal (GI) tract. Table 6.2 shows the number of and the rate at which patients experienced GI bleeding in the SAVAYSA 60 mg and warfarin treatment groups.
| SAVAYSA N = 5417 n (%/year) | Warfarin N = 5485 n (%/year) |
|
|---|---|---|
|
||
| Major Gastrointestinal (GI) Bleeding† | 205 (1.78) | 150 (1.27) |
| Upper GI | 123 (1.06) | 88 (0.74) |
| Lower GI‡ | 85 (0.73) | 64 (0.54) |
| GUSTO§ Severe GI bleeding | 16 (0.14) | 17 (0.14) |
| Fatal GI bleeding | 1 (< 0.1) | 2 (< 0.1) |
The rate of anemia-related adverse events was greater with SAVAYSA 60 mg than with warfarin (9.6% vs. 6.8%).
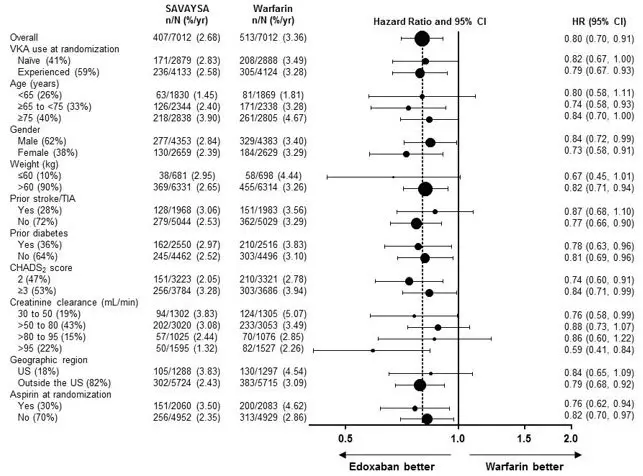
The comparative rates of major bleeding on SAVAYSA and warfarin were generally consistent among subgroups (see Figure 6.1). Bleeding rates appeared higher in both treatment arms (SAVAYSA and warfarin) in the following subgroups of patients: those receiving aspirin, those in the United States, those more than 75 years old and those with reduced renal function.
| Figure 6.1: Adjudicated Major Bleeding in the ENGAGE AF-TIMI 48* Study |
|---|
| Note: The figure above presents effects in various subgroups all of which are baseline characteristics and most of which were pre-specified. The 95% confidence limits that are shown do not take into account how many comparisons were made, nor do they reflect the effect of a particular factor after adjustment for all other factors. Apparent homogeneity or heterogeneity among groups should not be over-interpreted. |
|
|
|
Bleeding in Patients with DVT and/or PE in the Hokusai VTE Study
The major safety outcome was Clinically Relevant Bleeding, defined as the composite of Major and Clinically Relevant Non-Major (CRNM) Bleeding that occurred during or within three days of stopping study treatment. The incidence of Clinically Relevant Bleeding was lower in SAVAYSA than warfarin [HR (95% CI): 0.81 (0.71, 0.94); p = 0.004].
Table 6.3 shows the number of patients experiencing bleeding events in the Hokusai VTE Study.
| SAVAYSA (N = 4118) | Warfarin (N = 4122) |
|
|---|---|---|
| Abbreviations: N = number of patients in the modified intent-to-treat population; n = number of events; CRNM = clinically relevant non-major | ||
|
||
| Clinically Relevant Bleeding* (Major/CRNM), n (%) | 349 (8.5) | 423 (10.3) |
| Major Bleeding†, n (%) | 56 (1.4) | 66 (1.6) |
| Fatal bleeding | 2 (<0.1) | 10 (0.2) |
| Intracranial fatal | 0 (0.0) | 6 (0.1) |
| Non-fatal critical organ bleeding | 13 (0.3) | 25 (0.6) |
| Intracranial bleeding | 5 (0.1) | 12 (0.3) |
| Non-fatal non-critical organ bleeding | 41 (1.0) | 33 (0.8) |
| Decrease in Hb ≥ 2 g/dL | 40 (1.0) | 33 (0.8) |
| Transfusion of ≥ 2 units of RBC | 28 (0.7) | 22 (0.5) |
| CRNM Bleeding‡ | 298 (7.2) | 368 (8.9) |
| Any Bleed | 895 (21.7) | 1056 (25.6) |
Patients with low body weight (≤ 60 kg), CrCL ≤ 50 mL/min, or concomitant use of select P-gp inhibitors were randomized to receive SAVAYSA 30 mg or warfarin. As compared to all patients who received SAVAYSA or warfarin in the 60 mg cohort, all patients who received SAVAYSA or warfarin in the 30 mg cohort (n = 1452, 17.6% of the entire study population) were older (60.1 vs 54.9 years), more frequently female (66.5% vs 37.7%), more frequently of Asian race (46.0% vs 15.6%) and had more co-morbidities (e.g., history of bleeding, hypertension, diabetes, cardiovascular disease, cancer). Clinically relevant bleeding events occurred in 58/733 (7.9%) of the SAVAYSA patients receiving 30 mg once daily and 92/719 (12.8%) of warfarin patients meeting the above criteria.
In the Hokusai VTE study, among all patients the most common bleeding adverse reactions (≥ 1%) are shown in Table 6.4.
| SAVAYSA 60 mg (N = 4118) n (%) | Warfarin (N = 4122) n (%) |
|
|---|---|---|
|
||
| Bleeding ADRs* | ||
| Vaginal† | 158 (9) | 126 (7.1) |
| Cutaneous soft tissue | 245 (5.9) | 414 (10) |
| Epistaxis | 195 (4.7) | 237 (5.7) |
| Gastrointestinal bleeding | 171 (4.2) | 150 (3.6) |
| Lower gastrointestinal | 141 (3.4) | 126 (3.1) |
| Oral/pharyngeal | 138 (3.4) | 162 (3.9) |
| Macroscopic hematuria/urethral | 91 (2.2) | 117 (2.8) |
| Puncture site | 56 (1.4) | 99 (2.4) |
| Non-Bleeding ADRs | ||
| Rash | 147 (3.6) | 151 (3.7) |
| Abnormal liver function tests | 322 (7.8) | 322 (7.8) |
| Anemia | 72 (1.7) | 55 (1.3) |
Bleeding in Patients with VTE in the Hokusai VTE Cancer Study
The safety of SAVAYSA in patients with cancer and VTE was evaluated in the Hokusai VTE Cancer study [see Clinical Studies (14.2)]. The median duration of SAVAYSA exposure was 211 days (range, 2 to 423). The safety outcome was major bleeding that occurred during or within three days of stopping study treatment. The incidence of major bleeding was higher in the SAVAYSA arm than in the dalteparin arm [HR (95% CI): 2.00 (1.09, 3.66)].
Table 6.5 presents the bleeding results from the Hokusai VTE Cancer study.
| SAVAYSA (N = 522) | Dalteparin (N = 524) |
|
|---|---|---|
| Abbreviations: N = number of patients in the modified intent-to-treat population; n = number of events; CRNM = clinically relevant non-major | ||
|
||
| Major Bleeding*, n (%) | 32 (6.1%) | 16 (3.1%) |
| Fatal bleeding | 1 (0.2%)† | 2 (0.4%) |
| Intracranial | 0 | 1 (0.2%) |
| Lower gastrointestinal | 1 (0.2%) | 1 (0.2%) |
| Non-fatal critical organ bleeding | 5 (1%) | 6 (1.1%) |
| Intracranial bleeding | 2 (0.4%) | 2 (0.4%) |
| Non-fatal non-critical organ bleeding | 27 (5.2%) | 8 (1.5%) |
| Gastrointestinal | 22 (4.2%) | 4 (0.8%) |
| Upper gastrointestinal | 18 (3.4%) | 3 (0.6%) |
| Lower gastrointestinal | 3 (0.6%) | 1 (0.2%) |
| Decrease in Hb ≥ 2 g/dL | 28 (5.4%) | 11 (2.1%) |
| CRNM Bleeding‡, n (%) | 70 (13.4%) | 48 (9.2%) |
| Any Bleeding, n (%) | 137 (26.2%) | 104 (19.8%) |
In patients with GI cancer at randomization, major bleeding occurred in 13.2% (18/136) in the SAVAYSA group and 2.4% (3/125) in the dalteparin group. In patients without GI cancer at randomization, major bleeding occurred in 3.6% (14/386) in the SAVAYSA group and 3.3% (13/399) in the dalteparin group.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of SAVAYSA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and lymphatic system disorders: thrombocytopenia
Gastrointestinal disorders: abdominal pain
Immune system disorders: angioedema, hypersensitivity
Nervous system disorders: dizziness, headache
Skin and subcutaneous tissue disorders: urticaria
7. Drug Interactions
7.1 Anticoagulants, Antiplatelets, Thrombolytics, and SSRIs/SNRIs
Co-administration of anticoagulants, antiplatelet drugs, thrombolytics and SSRIs or SNRIs may increase the risk of bleeding. Promptly evaluate any signs or symptoms of blood loss if patients are treated concomitantly with anticoagulants, aspirin, other platelet aggregation inhibitors, and/or NSAIDs [see Warnings and Precautions (5.3)].
Long-term concomitant treatment with SAVAYSA and other anticoagulants is not recommended because of increased risk of bleeding [see Warnings and Precautions (5.3)]. Short term co-administration may be needed for patients transitioning to or from SAVAYSA [see Dosage and Administration (2.4)].
In clinical studies with SAVAYSA concomitant use of aspirin (low dose ≤ 100 mg/day) or thienopyridines, and NSAIDs was permitted and resulted in increased rates of Clinically Relevant Bleeding. Carefully monitor for bleeding in patients who require chronic treatment with low dose aspirin and/or NSAIDs [see Warnings and Precautions (5.3) and Clinical Pharmacology (12.3)].
As with other anticoagulants the possibility may exist that patients are at an increased risk of bleeding in case of concomitant use with SSRIs or SNRIs due to their reported effect on platelets [see Warnings and Precautions (5.3)].
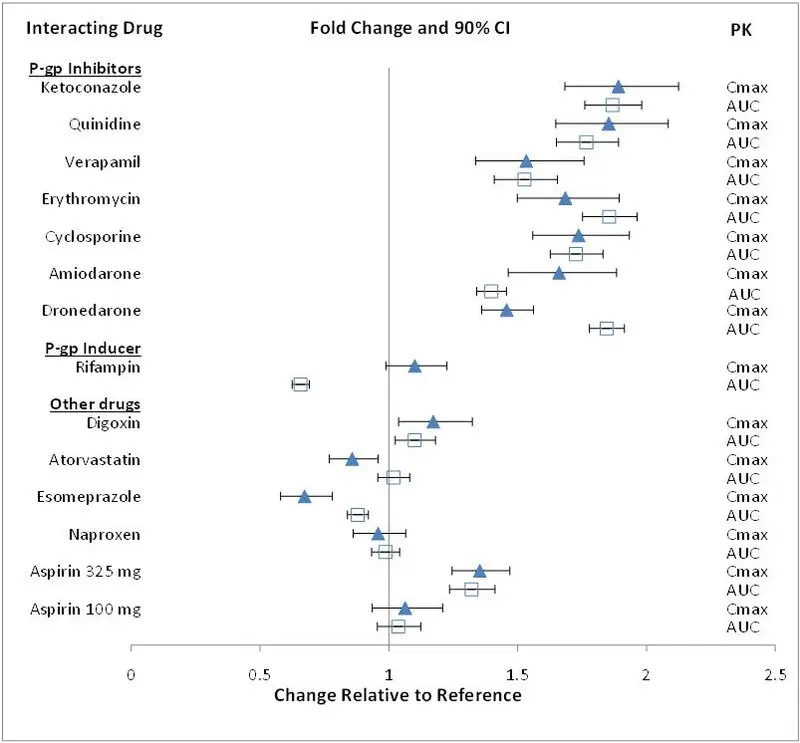
7.2 P-gp Inducers
Avoid the concomitant use of SAVAYSA with rifampin [see Clinical Pharmacology (12.3)].
8. Use In Specific Populations
8.3 Females and Males of Reproductive Potential
Females of reproductive potential requiring anticoagulation should discuss pregnancy planning with their physician.
The risk of clinically significant uterine bleeding, potentially requiring gynecological surgical interventions, identified with oral anticoagulants including SAVAYSA should be assessed in females of reproductive potential and those with abnormal uterine bleeding.
8.5 Geriatric Use
Of the total patients in the ENGAGE AF-TIMI 48 study, 5182 (74%) were 65 years and older, while 2838 (41%) were 75 years and older. In Hokusai VTE, 1334 (32%) patients were 65 years and older, while 560 (14%) patients were 75 years and older. In the Hokusai VTE Cancer Study, 539 (52%) patients were 65 years and older and 176 (17%) were 75 years and older. In clinical trials the efficacy and safety of SAVAYSA in elderly (65 years or older) and younger patients were similar [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14)].
8.6 Renal Impairment
Renal clearance accounts for approximately 50% of the total clearance of edoxaban. Consequently, edoxaban blood levels are increased in patients with poor renal function compared to those with higher renal function. Reduce SAVAYSA dose to 30 mg once daily in patients with CrCL 15-50 mL/min. There are limited clinical data with SAVAYSA in patients with CrCL < 15 mL/min; SAVAYSA is therefore not recommended in these patients. Hemodialysis does not significantly contribute to SAVAYSA clearance [see Dosage and Administration (2.1, 2.2) and Clinical Pharmacology (12.3)].
As renal function improves and edoxaban blood levels decrease, the risk for ischemic stroke increases in patients with NVAF [see Indications and Usage (1.1), Dosage and Administration (2.1), and Clinical Studies (14.1)].
8.7 Hepatic Impairment
The use of SAVAYSA in patients with moderate or severe hepatic impairment (Child-Pugh B and C) is not recommended as these patients may have intrinsic coagulation abnormalities. No dose reduction is required in patients with mild hepatic impairment (Child-Pugh A) [see Clinical Pharmacology (12.3)].
10. Overdosage
A specific reversal agent for edoxaban is not available. Overdose of SAVAYSA increases the risk of bleeding.
The following are not expected to reverse the anticoagulant effects of edoxaban: protamine sulfate, vitamin K, and tranexamic acid [see Warnings and Precautions (5.3)].
Hemodialysis does not significantly contribute to edoxaban clearance [see Pharmacokinetics (12.3)].
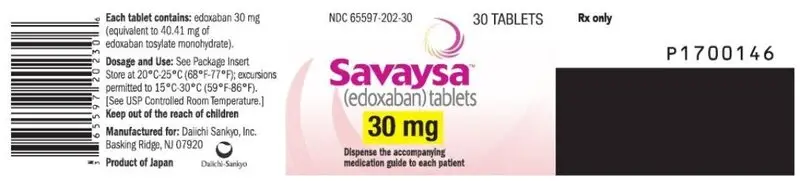
11. Savaysa Description
Edoxaban, a factor Xa inhibitor, is supplied as edoxaban tosylate monohydrate. The chemical name is N-(5-Chloropyridin-2-yl)-N'-[(1S,2R,4S)-4-(N,N-dimethylcarbamoyl)-2-(5-methyl-4,5,6,7-tetrahydro[1,3]thiazolo[5,4-c]pyridine-2-carboxamido)cyclohexyl] oxamide mono (4-methylbenzenesulfonate) monohydrate. Edoxaban tosylate monohydrate has the empirical formula C24H30ClN7O4S∙C7H8O3S∙H2O representing a molecular weight of 738.27. The chemical structure of edoxaban tosylate monohydrate is:
It is a white to pale yellowish-white crystalline powder. The solubility of edoxaban tosylate (pKa 6.7) decreases with increasing pH. It is slightly soluble in water, pH 3 to 5 buffer, very slightly soluble at pH 6 to 7; and practically insoluble at pH 8 to 9.
SAVAYSA is available for oral administration as a 60 mg, 30 mg, or 15 mg round shaped, film-coated tablet, debossed with product identification markings. Each 60 mg tablet contains 80.82 mg edoxaban tosylate monohydrate equivalent to 60 mg of edoxaban. Each 30 mg tablet contains 40.41 mg edoxaban tosylate monohydrate equivalent to 30 mg of edoxaban. Each 15 mg tablet contains 20.20 mg edoxaban tosylate monohydrate equivalent to 15 mg of edoxaban. The inactive ingredients are: mannitol, pregelatinized starch, crospovidone, hydroxypropyl cellulose, magnesium stearate, talc, and carnauba wax. The color coatings contain hypromellose, titanium dioxide, talc, polyethylene glycol 8000, iron oxide yellow (60 mg tablets and 15 mg tablets), and iron oxide red (30 mg tablets and 15 mg tablets).
12. Savaysa - Clinical Pharmacology
12.1 Mechanism of Action
Edoxaban is a selective inhibitor of FXa. It does not require antithrombin III for antithrombotic activity. Edoxaban inhibits free FXa, and prothrombinase activity and inhibits thrombin-induced platelet aggregation. Inhibition of FXa in the coagulation cascade reduces thrombin generation and reduces thrombus formation.
12.2 Pharmacodynamics
As a result of FXa inhibition, edoxaban prolongs clotting time tests such as prothrombin time (PT), and activated partial thromboplastin time (aPTT). Changes observed in PT, INR, and aPTT at the expected therapeutic dose, however, are small, subject to a high degree of variability and not useful in monitoring the anticoagulant effect of edoxaban. Following oral administration, peak pharmacodynamic effects are observed within 1-2 hours, which correspond with peak edoxaban concentrations (Cmax).
12.3 Pharmacokinetics
Edoxaban displays approximately dose-proportional pharmacokinetics for doses of 15 to 150 mg and 60 to 120 mg following single and repeat doses, respectively, in healthy subjects.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Edoxaban was not carcinogenic when administered daily to mice and rats by oral gavage for up to 104 weeks. The highest dose tested (500 mg/kg/day) in male and female mice was 3 and 6 times, respectively, the human exposure (AUC) at the human dose of 60 mg/day, and the highest doses tested in male (600/400 mg/kg/day) and female (200 mg/kg/day) rats were 8 and 14 times, respectively, the human exposure at the human dose of 60 mg/day.
Edoxaban and its human-specific metabolite, M-4, were genotoxic in in vitro chromosomal aberration tests but were not genotoxic in the in vitro bacterial reverse mutation (Ames test), in in vitro human lymphocytes micronucleus test, in in vivo rat bone marrow micronucleus test, in in vivo rat liver micronucleus test, and in in vivo unscheduled DNA synthesis tests.
Edoxaban showed no effects on fertility and early embryonic development in rats at doses of up to 1000 mg/kg/day (162 times the human dose of 60 mg/day normalized to body surface area).
14. Clinical Studies
14.1 Nonvalvular Atrial Fibrillation
The ENGAGE AF-TIMI 48 Study
The ENGAGE AF-TIMI 48 (NCT00781391) study was a multi-national, double-blind, non-inferiority study comparing the efficacy and safety of two SAVAYSA treatment arms (60 mg and 30 mg) to warfarin (titrated to INR 2.0 to 3.0) in reducing the risk of stroke and systemic embolic events in patients with NVAF. The non-inferiority margin (degree of inferiority of SAVAYSA to warfarin that was to be ruled out) was set at 38%, reflecting the substantial effect of warfarin in reducing strokes. The primary analysis included both ischemic and hemorrhagic strokes.
To enter the study, patients had to have one or more of the following additional risk factors for stroke:
- a prior stroke (ischemic or unknown type), transient ischemic attack (TIA) or non-CNS systemic embolism, or
- 2 or more of the following risk factors:
- –
- age ≥ 75 years,
- –
- hypertension,
- –
- heart failure, or
- –
- diabetes mellitus
A total of 21,105 patients were randomized and followed for a median of 2.8 years and treated for a median of 2.5 years. Patients in the SAVAYSA treatment arms had their dose halved (60 mg halved to 30 mg or 30 mg halved to 15 mg) if one or more of the following clinical factors were present: CrCL ≤ 50 mL/min, low body weight (≤ 60 kg) or concomitant use of specific P-gp inhibitors (verapamil, quinidine, dronedarone). Patients on antiretroviral therapy (ritonavir, nelfinavir, indinavir, saquinavir) as well as cyclosporine were excluded from the study. Approximately 25% of patients in all treatment groups received a reduced dose at baseline, and an additional 7% were dose-reduced during the study. The most common reason for dose reduction was a CrCL ≤ 50 mL/min at randomization (19% of patients).
Patients were well balanced with respect to demographic and baseline characteristics. The percentages of patients age ≥ 75 years and ≥ 80 years were approximately 40% and 17%, respectively. The majority of patients were Caucasian (81%) and male (62%). Approximately 40% of patients had not taken a Vitamin K Antagonist (VKA) (i.e., never took a VKA or had not taken a VKA for more than 2 months).
The mean patient body weight was 84 kg (185 lbs) and 10% of patients had a body weight of ≤ 60 kg. Concomitant diseases of patients in this study included hypertension (94%), congestive heart failure (58%), and prior stroke or transient ischemic attack (28%). At baseline, approximately 30% of patients were on aspirin and approximately 2% of patients were taking a thienopyridine.
Patients randomized to the warfarin arm achieved a mean TTR (time in therapeutic range, INR 2.0 to 3.0) of 65% during the course of the study.
The primary endpoint of the study was the occurrence of first stroke (either ischemic or hemorrhagic) or of a systemic embolic event (SEE) that occurred during treatment or within 3 days from the last dose taken. In the overall results of the study, shown in Table 14.1, both treatment arms of SAVAYSA were non-inferior to warfarin for the primary efficacy endpoint of stroke or SEE. However, the 30 mg (15 mg dose-reduced) treatment arm was numerically less effective than warfarin for the primary endpoint, and was also markedly inferior in reducing the rate of ischemic stroke. Based on the planned superiority analysis (ITT, which required p < 0.01 for success), statistical superiority of the 60 mg (30 mg dose-reduced) treatment arm compared to warfarin was not established in the total study population, but there was a favorable trend [HR (99% CI): 0.87 (0.71, 1.07)].
| Events | SAVAYSA 30 mg† (N = 7002) n (%/yr)‡ | SAVAYSA 60 mg† (N = 7012) n (%/yr)‡ | Warfarin (N = 7012) n (%/yr)‡ | SAVAYSA 30 mg vs. warfarin HR (CI)§ p-value | SAVAYSA 60 mg vs. warfarin HR (CI)§ p-value |
|---|---|---|---|---|---|
| Abbreviations: HR = Hazard Ratio versus Warfarin, CI = Confidence Interval, n = number of events, mITT = Modified Intent-to-Treat, N = number of patients in mITT population, SEE = Systemic Embolic Event, yr = year. | |||||
|
|||||
| First Stroke or SEE | 253 (1.6) | 182 (1.2) | 232 (1.5) | 1.07 (0.87, 1.31) p = 0.44 | 0.79 (0.63, 0.99) p = 0.017 |
| Ischemic Stroke | 225 (1.4) | 135 (0.9) | 144 (0.9) | 1.54 (1.25, 1.90) | 0.94 (0.75, 1.19) |
| Hemorrhagic Stroke | 18 (0.1) | 39 (0.3) | 75 (0.5) | 0.24 (0.14, 0.39) | 0.52 (0.36, 0.77) |
| Systemic Embolism | 10 (< 0.1) | 8 (< 0.1) | 13 (< 0.1) | 0.75 (0.33, 1.72) | 0.62 (0.26, 1.50) |
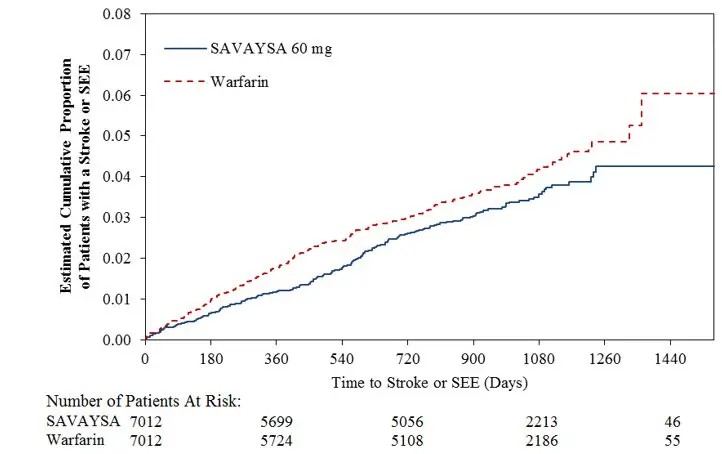
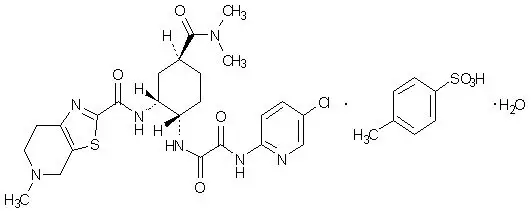
Figure 14.1 is a plot of the time from randomization to the occurrence of the first primary endpoint in all patients randomized to 60 mg SAVAYSA or warfarin.
| Figure 14.1: Kaplan-Meier Cumulative Event Rate Estimates for Primary Endpoint (first occurrence of stroke or SEE) (mITT*) |
|---|
|
|
|
The incidence rate of the primary endpoint of stroke or SEE in patients (N = 1776) treated with the 30 mg reduced dose of SAVAYSA because of a CrCL level ≤ 50 mL/min, low body weight ≤ 60 kg, or the concomitant use of a P-gp inhibitor drug, was 1.79% per year. Patients with any of these characteristics who were randomized to receive warfarin had an incidence rate of the primary endpoint of 2.21% per year [HR (95% CI): 0.81 (0.58, 1.13)].
In all randomized patients during the overall study period, the rates of CV death with SAVAYSA and warfarin were 2.74% per year vs. 3.17% per year, respectively [HR (95% CI): 0.86 (0.77, 0.97)].
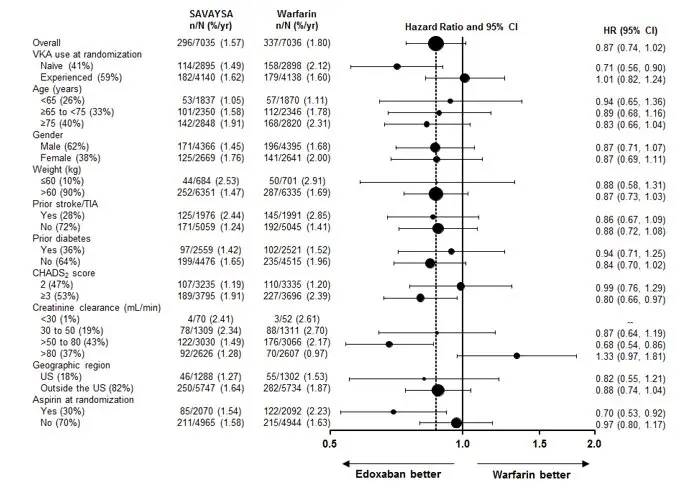
The results in the ENGAGE AF-TIMI 48 study for the primary efficacy endpoint for most major subgroups are displayed in Figure 14.2.
| Figure 14.2: ENGAGE AF-TIMI 48 Study: Primary Efficacy Endpoint by Subgroups (ITT Analysis Set) |
|---|
| Note: The figure above presents effects in various subgroups all of which are baseline characteristics and most of which were pre-specified. The 95% confidence limits that are shown do not take into account how many comparisons were made, nor do they reflect the effect of a particular factor after adjustment for all other factors. Apparent homogeneity or heterogeneity among groups should not be over-interpreted. |
|
|
The results of the ENGAGE AF-TIMI 48 study show a strong relationship between the blood levels of edoxaban and its effectiveness in reducing the rate of ischemic stroke. There was a 64% increase in the ischemic stroke rate in patients in the 30 mg treatment arm (including patients with dose reduced to 15 mg) compared to the 60 mg treatment arm (including patients with dose reduced to 30 mg). Approximately half of the SAVAYSA dose is eliminated by the kidney, and edoxaban blood levels are lower in patients with better renal function, averaging about 30% less in patients with CrCL of > 80 mL/min, and 40% less in patients with CrCL > 95 mL/min when compared to patients with a CrCL of > 50 to ≤ 80 mL/min. Given the clear relationship of dose and blood levels to effectiveness in the ENGAGE AF-TIMI 48 study, it could be anticipated that patients with better renal function would show a smaller effect of SAVAYSA compared to warfarin than would patients with mildly impaired renal function, and this was in fact observed.
Table 14.2 shows the results for the study primary efficacy endpoint of first stroke or SEE as well as the effects on ischemic and hemorrhagic stroke in the pre-randomization CrCL subgroups for SAVAYSA 60 mg (including 30 mg dose-reduced) and warfarin. There was a decreased rate of ischemic stroke with SAVAYSA 60 mg compared to warfarin in patients with CrCL > 50 to ≤ 80 mL/min [HR (95% CI): 0.63 (0.44, 0.89)]. In patients with CrCL > 80 to ≤ 95 mL/min the results for ischemic stroke slightly favor warfarin with a confidence interval that crosses 1.0 [HR (95% CI): 1.11 (0.58, 2.12)]. The rate of ischemic stroke was higher relative to warfarin in the patients with CrCL > 95 mL/min [HR (95% CI): 2.16 (1.17, 3.97)]. Pharmacokinetic data indicate that patients with CrCL > 95 mL/min had lower plasma edoxaban levels, along with a lower rate of bleeding relative to warfarin than patients with CrCL ≤ 95 mL/min. Consequently, SAVAYSA should not be used in patients with CrCL > 95 mL/min [see Dosage and Administration (2.1), Warnings and Precautions (5.1), Adverse Reactions (6.1), and Clinical Pharmacology (12.3)].
In patients with CrCL ≤ 95 mL/min, the SAVAYSA 60 mg (30 mg dose-reduced) treatment arm reduced the risk of stroke or SEE when compared to warfarin [HR (95% CI): 0.68 (0.55, 0.84)].
In the indicated population (CrCL ≤ 95 mL/min), during the overall study period, the rates of CV death with SAVAYSA and warfarin were 2.95% per year vs. 3.59% per year, respectively [HR (95% CI): 0.82 (0.72, 0.93)].
| STROKE TYPE Renal Function Subgroups* | Treatment Arm | n (N) | Event Rate (%/yr) | SAVAYSA 60 mg vs. Warfarin HR (95% CI) |
|---|---|---|---|---|
| Abbreviations: HR = Hazard Ratio versus Warfarin, CI = Confidence Interval, n = number of events, mITT = Modified Intent-to-Treat, N = number of patients in mITT population, yr = year. | ||||
|
||||
| PRIMARY ENDPOINT
(STROKE/SEE) |
||||
| ≤ 95 (Indicated Population) | Warfarin | 211 (5485) | 1.8 | 0.68 (0.55, 0.84) |
| SAVAYSA 60 mg | 142 (5417) | 1.2 | ||
| ≤ 50† | Warfarin | 50 (1356) | 2.0 | 0.90 (0.60, 1.34) |
| SAVAYSA 60 mg | 45 (1372) | 1.8 | ||
| > 50 to ≤ 80 | Warfarin | 135 (3053) | 2.0 | 0.53 (0.40, 0.70) |
| SAVAYSA 60 mg | 71 (3020) | 1.1 | ||
| > 80 to ≤ 95 | Warfarin | 26 (1076) | 1.0 | 1.05 (0.61, 1.82) |
| SAVAYSA 60 mg | 26 (1025) | 1.1 | ||
| > 95‡ | Warfarin | 21 (1527) | 0.6 | 1.87 (1.10, 3.17) |
| SAVAYSA 60 mg | 40 (1595) | 1.0 | ||
| ISCHEMIC STROKE | ||||
| ≤ 95 (Indicated Population) | Warfarin | 129 (5485) | 1.1 | 0.80 (0.62, 1.04) |
| SAVAYSA 60 mg | 102 (5417) | 0.9 | ||
| ≤ 50† | Warfarin | 28 (1356) | 1.1 | 1.11 (0.66, 1.84) |
| SAVAYSA 60 mg | 31 (1372) | 1.2 | ||
| > 50 to ≤ 80 | Warfarin | 83 (3053) | 1.2 | 0.63 (0.44, 0.89) |
| SAVAYSA 60 mg | 52 (3020) | 0.8 | ||
| > 80 to ≤ 95 | Warfarin | 18 (1076) | 0.7 | 1.11 (0.58, 2.12) |
| SAVAYSA 60 mg | 19 (1025) | 0.8 | ||
| > 95‡ | Warfarin | 15 (1527) | 0.4 | 2.16 (1.17, 3.97) |
| SAVAYSA 60 mg | 33 (1595) | 0.9 | ||
| HEMORRHAGIC STROKE | ||||
| ≤ 95 (Indicated Population) | Warfarin | 70 (5485) | 0.6 | 0.50 (0.33, 0.75) |
| SAVAYSA 60 mg | 34 (5417) | 0.3 | ||
| ≤ 50† | Warfarin | 18 (1356) | 0.7 | 0.66 (0.32, 1.36) |
| SAVAYSA 60 mg | 12 (1372) | 0.5 | ||
| > 50 to ≤ 80 | Warfarin | 45 (3053) | 0.7 | 0.38 (0.22, 0.67) |
| SAVAYSA 60 mg | 17 (3020) | 0.3 | ||
| > 80 to ≤ 95 | Warfarin | 7 (1076) | 0.3 | 0.76 (0.24, 2.38) |
| SAVAYSA 60 mg | 5 (1025) | 0.2 | ||
| > 95‡ | Warfarin | 6 (1527) | 0.2 | 0.98 (0.31, 3.05) |
| SAVAYSA 60 mg | 6 (1595) | 0.2 | ||
14.2 Treatment of Deep Vein Thrombosis and Pulmonary Embolism
SAVAYSA for the treatment of patients with deep vein thrombosis (DVT) and pulmonary embolism (PE) was studied in a multi-national, double-blind study (Hokusai VTE) (NCT00986154) which compared the efficacy and safety of SAVAYSA 60 mg orally once daily to warfarin (titrated to INR 2.0 to 3.0) in patients with acute symptomatic venous thromboembolism (VTE) (DVT or PE with or without DVT). All patients had VTE confirmed by appropriate diagnostic imaging at baseline and received initial heparin therapy with low molecular weight heparin (LMWH) or unfractionated heparin for at least 5 days [median LMWH/heparin treatment in the SAVAYSA 60 mg group was 7 days, and in the warfarin group it was 8.0 days] and until INR (sham or real) was ≥ 2.0 on two measurements. Blinded drug treatment in the warfarin arm was started concurrently with initial heparin therapy and in the SAVAYSA arm after discontinuation of initial heparin. Patients randomized to SAVAYSA received 30 mg once daily if they met one or more of the following criteria: CrCL 30 to 50 mL/min, body weight ≤ 60 kg, or concomitant use of specific P-gp inhibitors (verapamil and quinidine or the short-term concomitant administration of azithromycin, clarithromycin, erythromycin, oral itraconazole or oral ketoconazole). The edoxaban dosage regimen was to be returned to the regular dosage of 60 mg once daily at any time the subject is not taking the concomitant medication provided no other criteria for dose reduction are met. Other P-gp inhibitors were not permitted in the study. Patients on antiretroviral therapy (ritonavir, nelfinavir, indinavir, saquinavir) as well as cyclosporine were excluded from the Hokusai VTE study. The concomitant use of these drugs with SAVAYSA has not been studied in patients. The treatment duration was from 3 months up to 12 months, determined by investigator based on patient clinical features. Patients were excluded if they required thrombectomy, insertion of a caval filter, use of a fibrinolytic agent, or use of other P-gp inhibitors, had a creatinine clearance < 30 mL/min, significant liver disease, or active bleeding. The primary efficacy outcome was symptomatic VTE, defined as the composite of recurrent DVT, new non-fatal symptomatic PE, and fatal PE during the 12-month study period.
A total of 8292 patients were randomized to receive SAVAYSA or warfarin and were followed for a mean treatment duration of 252 days for SAVAYSA and 250 days for warfarin. The mean age was approximately 56 years. The population was 57% male, 70% Caucasian, 21% Asian, and about 4% Black. The presenting diagnosis was PE (with or without DVT) in 40.7% and DVT only in 59.3% of patients. At baseline, 27.6% of patients had temporary risk factors only (e.g., trauma, surgery, immobilization, estrogen therapy). Overall 9.4% had a history of cancer, 17.3% of the patients had an age ≥ 75 years and/or a body weight ≤ 50 kg, and/or a CrCL < 50 mL/min, and 31.4% of patients had NT-ProBNP ≥ 500 pg/mL.
Aspirin was taken as on treatment concomitant antithrombotic medication by approximately 9% of patients in both groups.
In the warfarin group, the median TTR (time in therapeutic range, INR 2.0 to 3.0) was 65.6%.
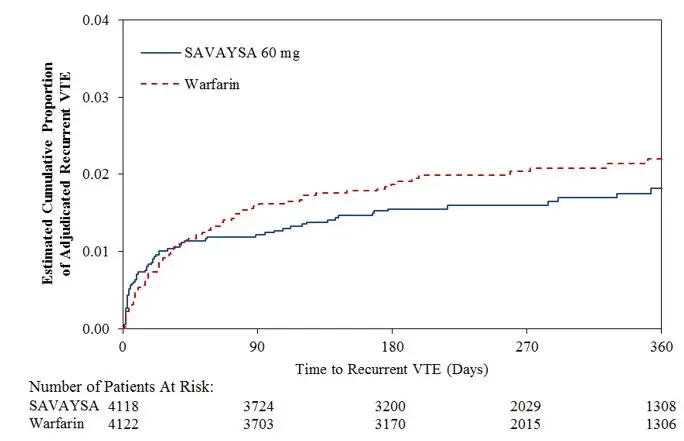
A total of 8240 patients (n = 4118 for SAVAYSA and n = 4122 for warfarin) received study drug and were included in the modified intent-to-treat (mITT) population. SAVAYSA was demonstrated to be non-inferior to warfarin for the primary endpoint of recurrent VTE [HR (95% CI): 0.89 (0.70, 1.13)] (Table 14.3, Figure 14.3).
| Primary Endpoint | SAVAYSA*
n/N (%) | Warfarin n/N (%) | SAVAYSA vs. Warfarin HR (95% CI) |
|---|---|---|---|
| Abbreviations: mITT = modified intent-to-treat; HR =hazard ratio vs. warfarin; CI =confidence interval; N = number of patients in mITT population; n = number of events | |||
|
|||
| All patients with symptomatic recurrent VTE† | 130/4118 (3.2) | 146/4122 (3.5) | 0.89 (0.70,1.13) |
| PE with or without DVT | 73/4118 (1.8) | 83/4122 (2.0) | - |
| Fatal PE and Death where PE cannot be ruled out | 24/4118 (0.6) | 24/4122 (0.6) | - |
| Non-fatal PE | 49/4118 (1.2) | 59/4122 (1.4) | - |
| DVT only | 57/4118 (1.4) | 63/4122 (1.5) | - |
| Index PE‡ patients with symptomatic recurrent VTE | 47/1650 (2.8) | 65/1669 (3.9) | - |
| Index DVT§ patients with symptomatic recurrent VTE | 83/2468 (3.4) | 81/2453 (3.3) | - |
Figure 14.3: Kaplan-Meier Cumulative Event Rate Estimates for Adjudicated Recurrent VTE (mITT analysis – on treatment)
16. How is Savaysa supplied
SAVAYSA (edoxaban) is supplied as round shaped, film-coated, non-scored tablets containing edoxaban tosylate equivalent to 60, 30 or 15 mg of SAVAYSA, packaged in bottles and blisters.
| NDC 65597-xxx-yy | ||||||||
|---|---|---|---|---|---|---|---|---|
| Strength | Color | Deboss | yy | |||||
| xxx | Bottle of | Blister of | ||||||
| 30 | 90 | 500 | 10 × 10* | 10 × 5† | ||||
|
||||||||
| 15 mg | orange | DSC L15 | 201 | 30 | - | - | - | - |
| 30 mg | pink | DSC L30 | 202 | 30 | 90 | 50 | 10 | 05 |
| 60 mg | yellow | DSC L60 | 203 | 30 | 90 | 50 | 10 | 05 |
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Advise patients of the following:
| MEDICATION GUIDE SAVAYSA (sa vaye' sah) (edoxaban) tablets |
|
|---|---|
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised.: 09/2021 |
What is the most important information I should know about SAVAYSA?
|
|
| What is SAVAYSA?
SAVAYSA is a prescription medicine used to:
|
|
| Who should not take SAVAYSA?
Do not take SAVAYSA if you currently have certain types of abnormal bleeding. |
|
Before taking SAVAYSA, tell your doctor about all of your medical conditions, including if you:
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Some of your other medicines may affect the way SAVAYSA works. Certain medicines may increase your risk of bleeding or stroke when taken with SAVAYSA. See "What is the most important information I should know about SAVAYSA?" Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine. |
|
How should I take SAVAYSA?
|
|
| What are the possible side effects of SAVAYSA? SAVAYSA can cause serious side effects. See " What is the most important information I should know about SAVAYSA?" The most common side effects in people who take SAVAYSA for nonvalvular atrial fibrillation include bleeding and low red blood cell count (anemia). The most common side effects in people who take SAVAYSA for deep vein thrombosis and pulmonary embolism include, bleeding, rash, abnormal liver function tests and low red blood cell count (anemia). Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
|
How should I store SAVAYSA?
|
|
| General information about the safe and effective use of SAVAYSA
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use SAVAYSA for a condition for which it was not prescribed. Do not give SAVAYSA to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or doctor for information about SAVAYSA that is written for health professionals. |
|
| What are the ingredients in SAVAYSA?
Active ingredient: edoxaban tosylate monohydrate Inactive ingredients: mannitol, pregelatinized starch, crospovidone, hydroxypropyl cellulose, magnesium stearate, talc, and carnauba wax. The color coatings contain hypromellose, titanium dioxide, talc, polyethylene glycol 8000, iron oxide yellow (60 mg tablets and 15 mg tablets), and iron oxide red (30 mg tablets and 15 mg tablets). Manufactured by: Daiichi Sankyo Co., LTD., Tokyo 103-8426, Japan Distributed by: Daiichi Sankyo, Inc., Basking Ridge, NJ 07920-2311 USA The brands listed above are trademarks of their respective owners. Copyright© 2021, Daiichi Sankyo, Inc. USMG-SAV-C8-0921-r102 For more information, call 1-877-437-7763 or go to https://savaysa.com/. |
|
| SAVAYSA
edoxaban tosylate tablet, film coated |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| SAVAYSA
edoxaban tosylate tablet, film coated |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
| SAVAYSA
edoxaban tosylate tablet, film coated |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Labeler - Daiichi Sankyo (068605067) |