Generic name: tofacitinib
Drug class: Antirheumatics
Dosage form: oral tablet, extended-release tablet, oral solution
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Tofacitinib
What is Xeljanz?
Xeljanz (tofacitinib) is an oral Janus kinase (JAK) inhibitor that may be used alone or with other medications to reduce inflammation associated with inflammatory and autoimmune conditions such as rheumatoid arthritis, psoriatic arthritis, and ulcerative colitis.
Xeljanz works by decreasing the activity of the immune system. It does this by blocking the activity of JAK enzymes (JAK1, JAK2, JAK3, TYK2) inside the cell – these enzymes are responsible for sending inflammatory signals in the body which are associated with cytokine release. By blocking these enzymes Xeljanz helps to decrease the immune reaction which causes rheumatoid arthritis, psoriatic arthritis, and ulcerative colitis.
Xeljanz may be used to treat the following conditions in adults who are unable to take or did not respond to one or more tumor necrosis factor (TNF) inhibitor medication(s)
- moderate to severe rheumatoid arthritis
- active psoriatic arthritis
- moderate to severe ulcerative colitis
- ankylosing spondylitis.
Xeljanz is also approved to treat polyarticular juvenile idiopathic arthritis in patients 2 years of age and older who have had an inadequate response or intolerance to one or more TNF blockers.
Xeljanz was FDA approved on November 6, 2012.
Warnings
Taking Xeljanz may increase your risk of life-threatening medical problems including serious infections, a hole or tear in your digestive tract, a heart attack or stroke, blood clots, or cancer.
Tell your doctor if you have a weak immune system, diabetes, chronic lung disease, or an infection such as hepatitis, tuberculosis, shingles, or HIV. Also tell your doctor if you've ever had diverticulitis, an ulcer in your stomach or intestines, cancer, a kidney transplant, heart problems, or a history of smoking, heart attack, stroke, or blood clots.
Call your doctor right away if you have a fever, night sweats, constant tiredness, weight loss, stomach pain, diarrhea or changes in bowel habits, trouble breathing, wheezing, a severe cough, or lumps in your neck, armpits, or groin.
Seek emergency medical help if you have sudden shortness of breath, chest pain spreading to your neck or arms, nausea, severe dizziness, a cold sweat, weakness on one side of your body, slurred speech, or pain, redness, or swelling in an arm or leg.
The use of Xeljanz in combination with biologic DMARDs or potent immunosuppressants such as azathioprine and cyclosporine is not recommended.
Xeljanz XR (extended-release tablets) are not interchangeable or substitutable with Xeljanz Oral Solution.
Xeljanz should not be started in patients with an absolute lymphocyte count less than 500 cells/mm3, absolute neutrophil counts (ANC) <1000 cells/mm3, or hemoglobin <9 g/dL.
Do not use in patients with severe hepatic impairment. Avoid use during an active serious infection, including localized infections.
Regular laboratory monitoring is recommended due to potential changes in lymphocytes, neutrophils, hemoglobin, liver enzymes, and lipids.
How should I take Xeljanz
Take Xeljanz exactly as prescribed by your doctor. Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose.
You may take Xeljanz with or without food.
Swallow the extended-release tablet whole and do not crush, chew, or break it.
Measure liquid medicine with the supplied measuring device (not a kitchen spoon).
Doses are based on weight in children and teenagers. Your child's dose may change if the child gains or loses weight.
A safe dose of Xeljanz is not the same for all conditions. Avoid medication errors by using only the form and strength your doctor prescribes.
You may get infections more easily, even serious or fatal infections. You will need frequent medical tests.
If you've ever had shingles (herpes zoster) or hepatitis B or C, using Xeljanz can cause these viruses to become active or get worse.
Part of a tablet shell may appear in your stool but this will not make the medicine less effective.
Store this medicine in the original container at room temperature, away from moisture, heat, and light. Throw away any unused liquid after 60 days.
Dosing information
Adults with Rheumatoid Arthritis, Psoriatic Arthritis, or Ankylosing Spondylitis
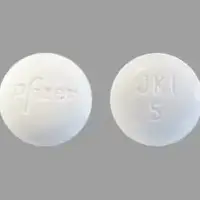
- Immediate-release tablets: 5 mg orally twice a day.
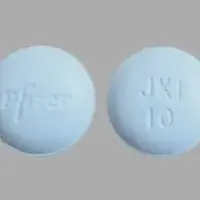
- Extended-release tablets: 11 mg orally once a day.
Reduce dosage to 5mg once daily in those with moderate to severe renal impairment or moderate hepatic impairment.
Psoriatic arthritis: use in combination with nonbiologic DMARDs.
Adults with Ulcerative Colitis
Immediate-Release Tablets:
- Induction: 10 mg orally twice a day for at least 8 weeks
- Maintenance: 5 mg orally twice a day.
Extended-Release Tablets:
- Induction: 22 mg orally once a day for at least 8 weeks
- Maintenance: 11 mg orally once a day.
If needed, induction dosages may be continued for up to 16 weeks; if adequate therapeutic response is not achieved after 16 weeks, the induction dosage should be discontinued.
For patients with loss of response during maintenance therapy, consider 10 mg orally twice a day (immediate-release tablets) or 22 mg orally once a day (extended-release tablets) for a short duration. Use the lowest effective dose needed to maintain a response.
Juvenile Idiopathic Arthritis in Children 2 Years and Older
Oral solution:
- Weight 10 to < 20 kg: 3.2 mg orally twice a day
- Weight 20 to < 40 kg: 4 mg orally twice a day
- Weight at least 40 kg: 5 mg orally twice a day.
Immediate-release tablets:
- Weight at least 40 kg: 5 mg orally twice a day.
Before Taking
Tell your doctor if you've had:
-
a weak immune system or chronic infection (such as tuberculosis, shingles, HIV, or hepatitis);
-
any type of cancer;
-
kidney disease, a kidney transplant, or if you are on dialysis;
-
diverticulitis, an ulcer in your stomach or intestines;
-
heart problems;
-
a heart attack, stroke, or blood clot;
-
high cholesterol; or
-
if you've ever smoked.
Tell your doctor if you've been sick with signs of infection, such as fever, chills, muscle aches, cough, trouble breathing, skin sores, diarrhea, or painful urination.
Tell your doctor if you've had or been exposed to tuberculosis, or if you recently traveled. Some infections are more common in certain parts of the world, and you may have been exposed during travel.
Also to make sure Xeljanz is safe for you, tell your doctor if you have ever had:
-
liver disease (especially hepatitis B or C);
-
chronic lung disease;
-
diabetes; or
-
if you are scheduled to receive any vaccine.
Using Xeljanz may increase your risk of developing certain cancers, such as lymphoma or lung cancer. Ask your doctor about this risk.
Tell your doctor if you are pregnant or plan to become pregnant. Having rheumatoid arthritis or ulcerative colitis during pregnancy may increase the risk of premature birth or low birth weight. The benefit of treating these conditions with Xeljanz may outweigh any risks to the baby. If you become pregnant while taking Xeljanz, your name may be recorded on a pregnancy registry to track the effects of Xeljanz on the baby.
If you are a woman, Xeljanz may affect your fertility and your ability to have children during treatment and in the future.
Do not breastfeed while you are using this medicine, and for at least 18 hours after your last dose (36 hours if you take extended-release tablets). If you use a breast pump during this time, do not feed the milk to your baby.
Do not give this medicine to a child without medical advice. The extended-release tablets are not approved for use by anyone younger than 18 years old.
How do I take Xeljanz?
Take Xeljanz exactly as prescribed by your doctor. Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose.
You may take Xeljanz with or without food.
Swallow the extended-release tablet whole and do not crush, chew, or break it.
Measure liquid medicine with the supplied measuring device (not a kitchen spoon).
Doses are based on weight in children and teenagers. Your child's dose may change if the child gains or loses weight.
What happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while using Xeljanz?
Avoid receiving a "live" vaccine. Live vaccines include measles, mumps, rubella (MMR), rotavirus, typhoid, yellow fever, varicella (chickenpox), and zoster (shingles).
Xeljanz side effects
Get emergency medical help if you have signs of an allergic reaction to Xeljanz, such as hives; difficulty breathing; swelling of your face, lips, tongue, or throat.
Some people taking Xeljanz have developed heart attacks, strokes, or serious blood clots. Stop taking this medicine and seek emergency medical attention if you have:
-
sudden shortness of breath;
-
chest pain or pressure that may spread to your jaw, shoulder, arms, or back;
-
nausea, vomiting, cold sweat;
-
a light-headed feeling, like you might pass out;
-
weakness on one side of your body;
-
slurred speech, drooping on one side of your mouth; or
-
pain, swelling, or redness in an arm or a leg.
Xeljanz may cause serious side effects. Call your doctor at once if you have:
-
fever, chills, night sweats, constant tiredness;
-
wheezing, trouble breathing, severe or worsening cough;
-
increased urination, pain or burning when you urinate;
-
unexplained weight loss;
-
lumps in your neck, armpits, or groin;
-
signs of shingles - flu-like symptoms, tingly or painful blistering rash on one side of your body;
-
a hole (perforation) in your digestive tract - fever, severe stomach pain, diarrhea or changes in bowel habits; or
-
signs of hepatitis - loss of appetite, vomiting, stomach pain (upper right side), dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes).
Common Xeljanz side effects may include:
-
skin rash, shingles
- upper respiratory tract infection or cold symptoms such as stuffy nose, sneezing, sore throat
-
increased blood pressure
- diarrhea
-
abnormal blood tests
- elevated cholesterol levels
-
fever
-
headache
-
nausea, or vomiting.
Patients receiving Xeljanz XR may notice an inert tablet shell passing in the stool or via colostomy. The active medication has already been absorbed by the time the inert tablet shell is seen.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
See more: Xeljanz Side EffectsWhat other drugs will affect Xeljanz?
Sometimes it is not safe to use certain medications at the same time. Some drugs can affect your blood levels of other drugs you take, which may increase side effects or make the medications less effective.
Tell your doctor about all your current medicines. Many drugs can interact with tofacitinib, especially:
-
azathioprine;
-
cyclosporine
-
moderate CYP3A4 inhibitors coadministered with strong CYP2C19 inhibitors (eg, fluconazole)
-
strong CYP3A4 inducers (eg, rifampin)
-
strong CP3A4 inhibitors (such as ketoconazole)
-
tacrolimus
-
other drugs to treat arthritis or ulcerative colitis - abatacept, adalimumab, anakinra, certolizumab, etanercept, golimumab, infliximab, rituximab, secukinumab, tocilizumab, ustekinumab, vedolizumab.
This list is not complete and many other drugs may interact with tofacitinib. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.